Gallbladder removal is one of the most common surgical procedures worldwide, especially for people dealing with gallstones, inflammation, or other gallbladder-related conditions. Although the operation is routine and generally safe, many patients still wonder what changes to expect once the organ is gone.
The gallbladder is small, but it plays a valuable role in digestion. Understanding what it does — and how your body adapts without it — can help you feel more prepared for recovery and long-term health after surgery.
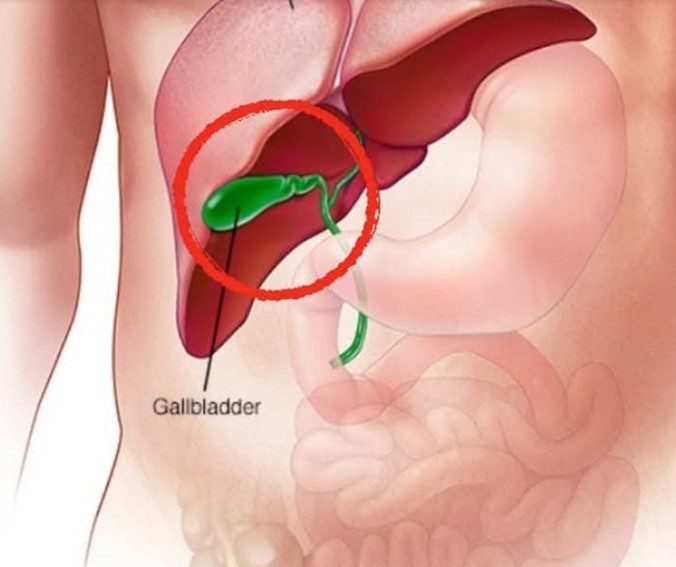
What the Gallbladder Does

The gallbladder is a small, pear-shaped organ located beneath the liver. Its main job is to store and concentrate bile, a digestive fluid the liver produces. When you eat, especially meals containing fat, the gallbladder releases bile into the small intestine to help break food down.
Even though the organ is small, its role in fat digestion often becomes more noticeable once it is removed. To understand why, it helps to review the most common gallbladder problems that lead to surgery.
Common Gallbladder Conditions
Several conditions can interfere with the gallbladder’s ability to function properly. According to medical experts, the most frequently diagnosed issues include:
Gallstones
Gallstones are hardened deposits made from bile components. They can range in size from tiny grains to larger stones. Many people never experience symptoms, but for others, gallstones can block bile flow and trigger pain, nausea, or inflammation.
Cholecystitis
If a gallstone blocks the cystic duct — the tube that allows bile to leave the gallbladder — the organ can become inflamed. Cholecystitis often causes severe pain, fever, and tenderness. In many cases, it requires surgery to prevent complications.
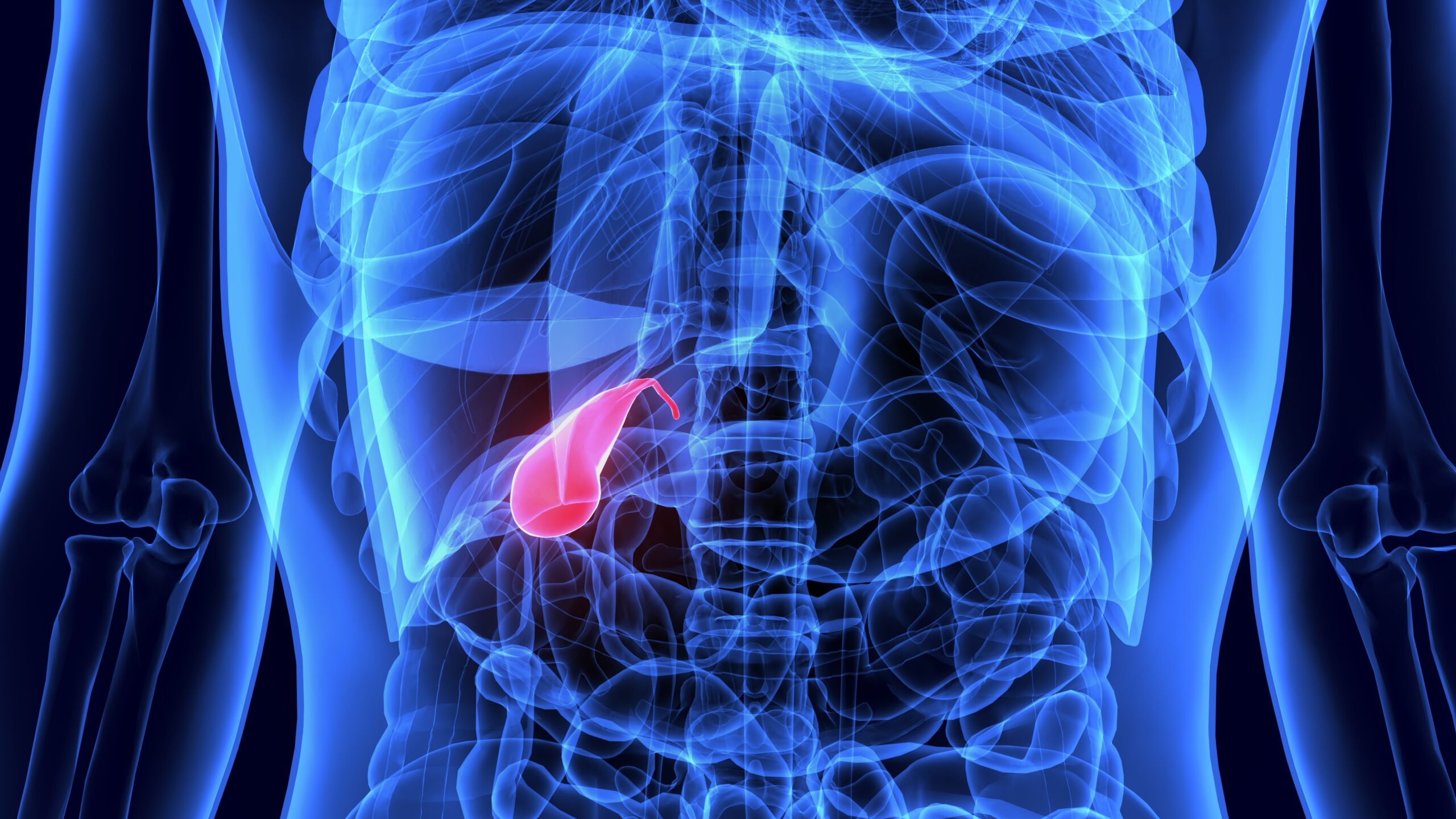
Gallstone Pancreatitis
Sometimes a gallstone travels into the common bile duct and obstructs the pancreatic duct. This blockage can cause inflammation of the pancreas, a condition that often requires hospitalization.
Gallbladder Cancer
Gallbladder cancer is rare, but because early symptoms often resemble other digestive issues, it can be difficult to detect in early stages. Persistent pain or digestive changes should always be checked by a medical professional.
Signs Your Gallbladder May Be Struggling
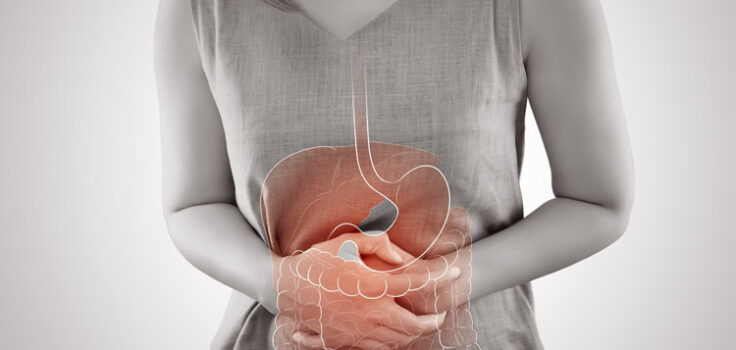
Gallbladder problems can present in several ways, though not everyone experiences all symptoms. Common signs include:
-
Discomfort in the upper right abdomen
-
Pain in the upper middle abdomen
-
Pain that spreads to the right shoulder or back
-
Discomfort after eating fatty meals
-
Nausea or vomiting
-
Fever or chills
-
Changes in urine or stool color
-
Jaundice (yellowing of the skin or eyes)
Any of these symptoms should prompt a visit to a healthcare provider for evaluation and testing.
What Happens After Gallbladder Removal
The liver continues producing bile even after the gallbladder is gone. The difference is that bile no longer has a storage area — it instead flows directly into the small intestine in a slow, continuous stream.
For most people, this adjustment is smooth. The digestive system adapts, and life returns to normal. However, some temporary changes are common in the first few weeks or months following surgery.
Changes in Fat Digestion
Since bile is no longer released in concentrated bursts, high-fat meals may feel more difficult to digest. This can lead to temporary symptoms such as:
-
Bloating
-
Cramping
-
Loose stools
-
Gas
-
Discomfort after eating rich or greasy foods
These effects usually improve as the body gets used to its new way of processing fats.
Bile Acid Diarrhea
A small portion of patients experience bile acid diarrhea — loose stools caused by bile irritating the lining of the intestines. This is typically temporary and can often be managed through diet adjustments or medications if needed.
Changes in Bowel Habits
For some people, bowel movements become more frequent or softer for a period after surgery. Others experience little to no change. Each person’s recovery is different, but most digestive patterns stabilize over time.
Diet Recommendations After Gallbladder Surgery
There is no strict, universal diet required after gallbladder removal, but making thoughtful choices can ease recovery. Medical organizations such as the Mayo Clinic offer general guidelines to help patients support digestion during the adjustment period.
1. Reduce Fat Intake
Foods that may be harder to digest include:
-
Fried foods
-
Fatty cuts of meat
-
Butter-heavy dishes
-
Rich sauces and gravies
Avoiding these for at least the first week — and reintroducing them slowly — can help reduce discomfort.
2. Increase Fiber Gradually
Fiber supports healthy digestion, but it should be added slowly to avoid gas or bloating. Whole grains, fruits, vegetables, and legumes can help regulate bowel movements.
3. Eat Smaller, More Frequent Meals
Large meals can overwhelm the digestive system during early recovery. Smaller portions spread throughout the day are easier to process.
4. Stay Well Hydrated
Water, herbal tea, and electrolyte-rich broths support digestion and help replace fluids if diarrhea occurs.
5. Limit Foods That May Worsen Diarrhea
Some items may irritate the digestive tract temporarily, such as:
-
Caffeine
-
High-fat dairy
-
Sugary foods
-
Spicy dishes
These can be reintroduced slowly as symptoms improve.
Most doctors recommend starting with light foods — such as soups, crackers, broths, oatmeal, and plain rice — before transitioning to a balanced diet. Over time, many patients find they can return to their usual meals with only minor adjustments.
Long-Term Outlook After Gallbladder Removal

The encouraging news is that living without a gallbladder does not prevent people from leading normal, healthy lives. The liver continues doing the majority of the work, and the digestive system adapts quickly.
Most long-term changes are mild, and many patients report feeling better once gallbladder symptoms are gone. Within a few months, the body usually settles into a stable rhythm, making digestion feel natural again.
Maintaining a balanced diet, staying active, and managing portion sizes can support overall digestive health — both before and after surgery.
When to Contact a Doctor After Surgery
While most people recover smoothly, medical guidance is important if you experience:
-
Severe abdominal pain
-
Persistent vomiting
-
Fever
-
Jaundice
-
Prolonged diarrhea
These may indicate complications or unrelated issues that require evaluation.
A Manageable Transition Toward Better Health
Gallbladder removal can feel like a major change, but for the vast majority of patients, it becomes just another chapter in their health journey. Digestive patterns may shift temporarily, but the body adapts well, and discomfort typically improves with time.
By making thoughtful food choices, staying hydrated, and listening to your body, recovery can feel smooth — and many people find relief from the painful symptoms that led them to surgery in the first place.
If you’ve been through this procedure, sharing your experience can help others feel supported as they navigate the transition.
Sources
-
Cleveland Clinic – Information on gallbladder conditions and symptoms
-
Mayo Clinic – Post-surgery dietary guidance and digestive health recommendations
-
Johns Hopkins Medicine – Overview of gallbladder removal and recovery steps