In recent years, health experts have emphasized the importance of awareness around human papillomavirus (HPV). It is one of the most common viral infections worldwide, affecting both men and women. Yet, conversations often focus only on women’s health, overlooking the fact that men, too, are impacted by HPV and its potential long-term consequences.
HPV is often referred to as a “silent” virus. Most people do not realize they have it because symptoms rarely appear. However, its presence can still cause health issues later in life. By increasing awareness, encouraging vaccination, and practicing preventive measures, men can significantly reduce their risks while also protecting their partners.
This article takes a closer look at what HPV is, how it spreads, why it matters for men, and the proactive steps that every individual can take to safeguard their health.
What Is HPV?
HPV stands for human papillomavirus, a group of more than 200 related viruses. Some types are considered low-risk and may cause mild skin issues, while others are classified as high-risk and are linked to certain cancers.
The Centers for Disease Control and Prevention (CDC) estimates that almost every sexually active person will be exposed to HPV at some point in life. While the body’s immune system often clears the infection naturally within one to two years, persistent strains can lead to more serious health outcomes.
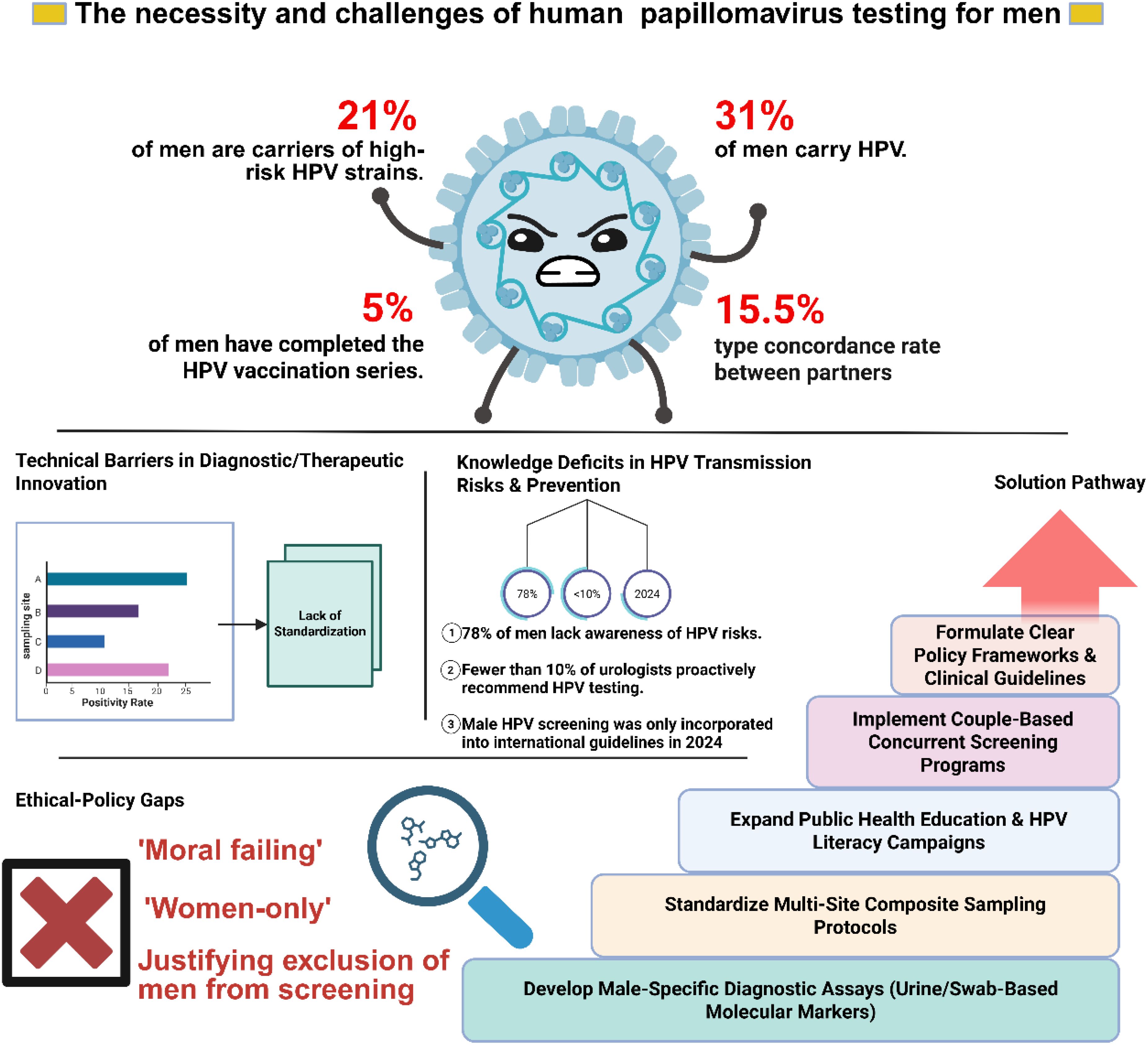
Why Men Should Be Concerned
For men, HPV has been connected to:
-
Throat and mouth conditions, caused by specific high-risk strains.
-
Skin growths that can appear in sensitive areas.
-
Increased cancer risk in rare cases, particularly anal or oropharyngeal cancers.
The fact that HPV is so widespread makes it not only a personal health issue but also a public health priority.
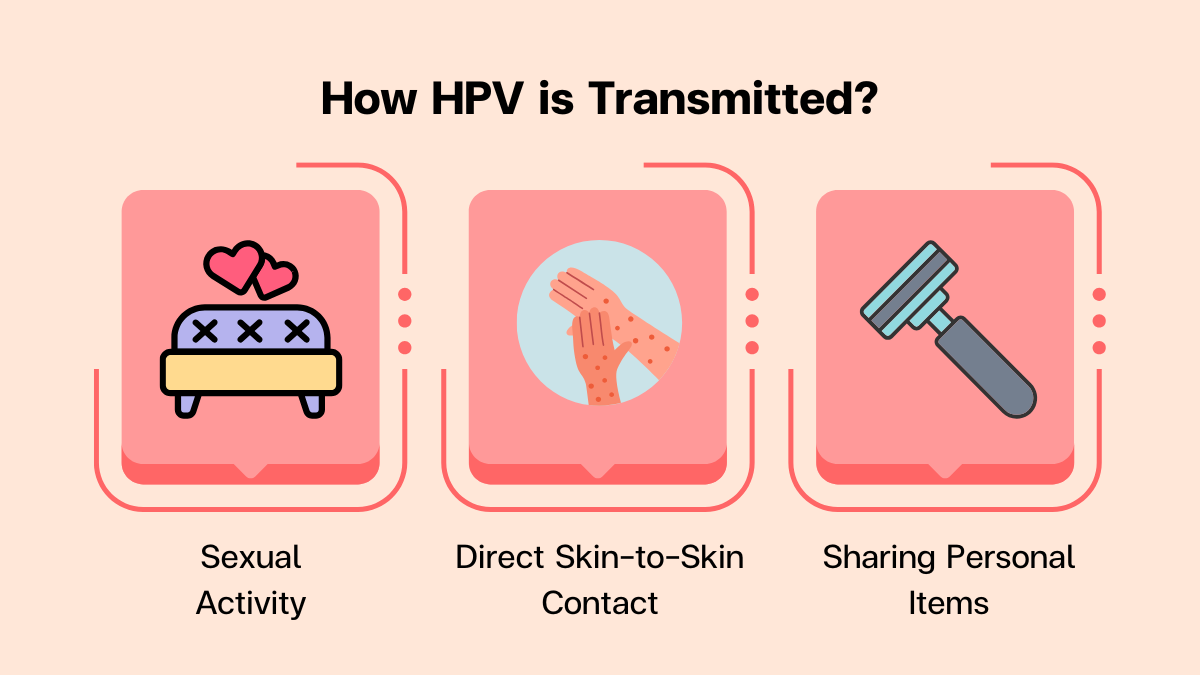
How HPV Spreads
One of the reasons HPV is so common is because it spreads easily through close skin-to-skin contact. Unlike some other infections, HPV does not require the exchange of bodily fluids to transmit. Even when no visible symptoms are present, the virus can still pass from one person to another.
This silent nature makes HPV difficult to track and prevent without proactive measures. Many people may not realize they carry the virus until years later, when related health problems arise.
The Link Between Lifestyle and HPV Risk
While HPV can affect anyone, research suggests that risk factors increase with greater exposure. Individuals with multiple close relationships over time are statistically more likely to encounter someone carrying a high-risk strain.
A study published in the journal Sexually Transmitted Diseases found a clear correlation between the number of partners reported and the likelihood of HPV exposure. However, it’s crucial to emphasize: even one relationship can result in exposure.
The more often the body encounters different strains, the harder it becomes for the immune system to eliminate them, which increases the chance of long-term persistence.
Symptoms and Potential Health Risks in Men
HPV is often symptomless, which is why regular health awareness is critical. When symptoms do occur, they may include:
-
Small skin growths in sensitive areas.
-
Respiratory papillomatosis, a rare condition where growths develop in the airways.
-
Oropharyngeal cancers, which affect the throat, tongue, or tonsils.
Most infections do not develop into serious illnesses. Still, because high-risk strains can cause severe health consequences, prevention and monitoring remain important.
The Emotional Side of HPV
Beyond physical symptoms, HPV can also carry an emotional toll. Men who test positive may feel anxiety, confusion, or shame. These feelings are often rooted in stigma and misinformation.
Why Emotional Awareness Matters
-
Reducing stigma: Understanding that HPV is extremely common helps remove unnecessary shame.
-
Encouraging openness: Talking about health status with partners promotes trust and shared responsibility.
-
Supporting mental health: Education and counseling can help individuals cope with the diagnosis without panic.
Prevention Strategies for Men
1. Vaccination
Perhaps the most effective tool against HPV is vaccination. Vaccines like Gardasil 9 protect against the strains most commonly linked to cancers and other complications.
-
Recommended age: Health authorities advise vaccination beginning at ages 11–12.
-
Catch-up vaccination: Men up to age 45 can still benefit, especially if they have not previously been exposed to certain strains.
-
Effectiveness: The vaccine has been proven safe and highly effective in preventing both low-risk and high-risk types of HPV.
2. Practicing Safer Behaviors
Using protection during close contact significantly reduces the likelihood of transmission, though it does not guarantee complete protection. This is because HPV can spread through areas not covered.
3. Regular Health Checkups
There is currently no routine test for HPV in men. However, doctors can detect visible symptoms and offer screenings for other related conditions. Staying consistent with checkups ensures early detection if problems arise.
4. Strengthening the Immune System
A healthy immune system is often able to clear HPV naturally. Maintaining good nutrition, exercising regularly, managing stress, and avoiding smoking all contribute to a stronger immune response.
5. Honest Communication
Discussing personal health openly with partners helps set expectations and builds mutual responsibility. Clear communication reduces stigma and helps everyone involved make informed decisions.
Common Myths About HPV
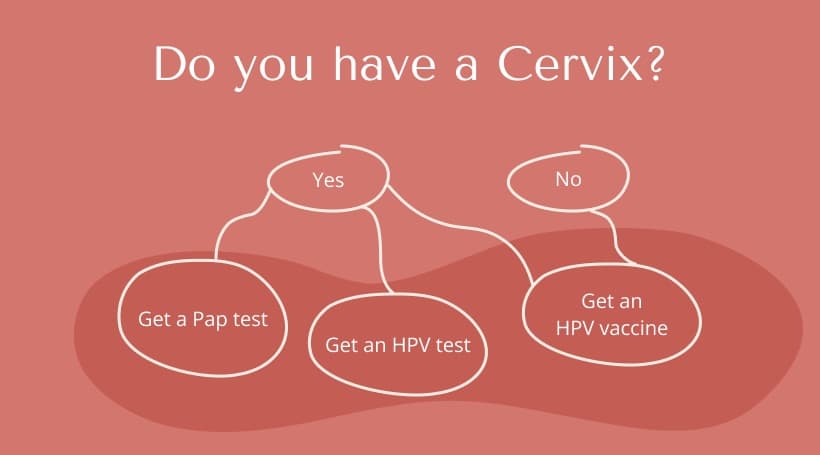
Myth 1: HPV only affects women.
Truth: Men can also experience HPV-related health problems and play an equal role in prevention.
Myth 2: If I don’t see symptoms, I don’t have it.
Truth: Many infections are symptomless, but the virus can still be present and transmissible.
Myth 3: Only people with “risky” lifestyles get HPV.
Truth: HPV is so common that nearly everyone will encounter it at some point, regardless of lifestyle.
Myth 4: Vaccines are unnecessary for men.
Truth: Vaccination benefits both men and women, lowering the overall circulation of the virus.
FAQs About HPV in Men
Q1: Can men be tested for HPV?
Currently, there is no widely available HPV screening test for men. Doctors rely on visual checks and related cancer screenings.
Q2: Does HPV always cause cancer?
No. Most infections clear naturally and never lead to cancer. Only persistent high-risk strains pose a concern.
Q3: If vaccinated, am I completely protected?
The vaccine covers the most common harmful strains but not every single type. Vaccinated individuals should still maintain healthy practices.
Q4: How long does HPV stay in the body?
For many, the immune system clears HPV within 1–2 years. Some infections, however, may persist longer and require medical attention.
Q5: Can HPV return after clearing?
Reinfection is possible, especially if exposed to new strains. Vaccination helps reduce this risk.
Long-Term Outlook: Living With HPV
The encouraging news is that most HPV infections do not cause lasting harm. With proactive care—vaccination, safer practices, and regular medical checkups—men can significantly lower their risks.
Living with HPV awareness does not mean living in fear. Instead, it means staying informed, making preventive choices, and supporting broader public health efforts to reduce transmission.
Final Thoughts
HPV is one of the most common viruses worldwide, and men play a vital role in prevention. By staying proactive—through vaccination, regular health monitoring, and open communication—men not only protect themselves but also contribute to healthier communities.
Awareness, education, and prevention are the most powerful tools in the fight against HPV. By treating it as a public health conversation rather than a taboo topic, society can reduce stigma and encourage responsible choices.
In the end, HPV does not have to disrupt health or relationships. With the right knowledge and steps, it is a challenge that can be managed, controlled, and largely prevented.
