Cervical cancer usually develops slowly. In many cases, it starts with long-lasting infection from high-risk human papillomavirus (HPV), and the changes in cervical cells can take years to progress. That slow timeline is exactly why prevention works: vaccination, screening, and early treatment can stop problems long before they become serious.
One thing that gets overlooked in family conversations is that a woman’s cervical health isn’t shaped by her actions alone. In long-term relationships, everyday habits inside the home—especially around sexual health, smoking, and medical follow-through—can quietly raise risk. Often it isn’t malice. It’s complacency, misinformation, and the “we’ll deal with it later” mindset.

Below are three relationship habits that can unintentionally increase risk over time—and what couples can do instead.
Habit 1: Treating Sexual Health as “Her Problem”
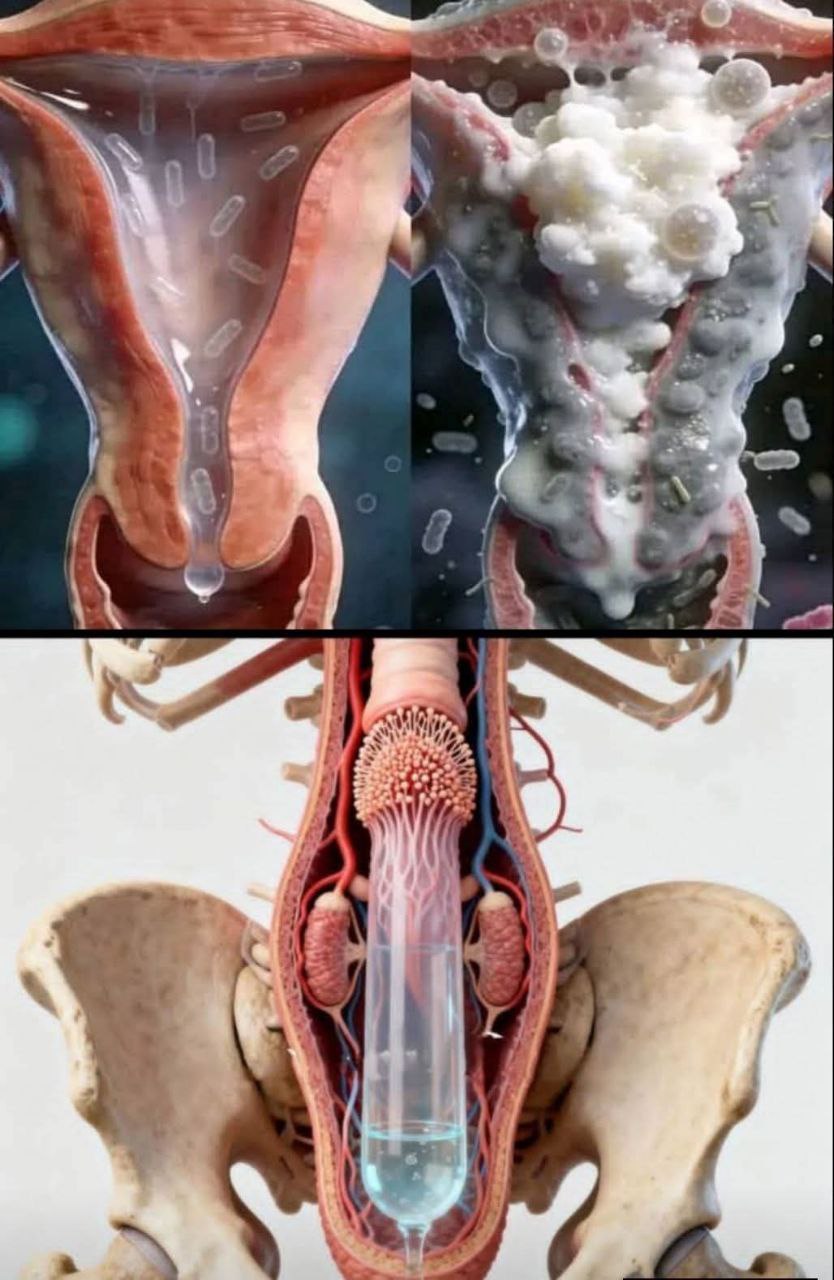
HPV is extremely common, and many people who carry it have no symptoms. A partner can carry or transmit HPV without knowing it, and “no symptoms” does not mean “no risk.” In a portion of cases, HPV can persist and increase the likelihood of precancerous changes in the cervix. (CDC)
Where couples go wrong is not the existence of HPV—it’s the attitude around prevention:
-
Avoiding conversations about sexual health history
-
Assuming that being in a committed relationship automatically equals zero risk
-
Dismissing HPV vaccination as “only for teenagers” or “not necessary now”
-
Ignoring follow-up when a partner has abnormal results or ongoing infections
What to do instead (practical and non-judgmental):
-
Talk like a team. If one partner gets an abnormal cervical screening result, treat it as a shared health priority, not an individual burden.
-
Consider HPV vaccination if eligible. Vaccination is one of the most effective prevention tools against HPV-related cancers. Policies and age guidance vary by country, but the point is: ask a clinician rather than assuming it’s “too late.” (World Health Organization)
-
Respect medical follow-up. If screening shows abnormalities, timely follow-up is how cervical cancer is prevented—not feared.
This isn’t about blaming husbands for HPV. It’s about dropping the myth that silence equals safety.
Habit 2: Smoking Indoors or Minimizing Secondhand Smoke
Smoking doesn’t just affect the person holding the cigarette. Secondhand smoke exposes family members to a mix of toxins that can weaken immune defenses. For cervical health, that matters because a strong immune system is one of the factors that helps the body clear HPV infections. Studies have linked smoking and passive smoke exposure with higher likelihood of cervical abnormalities and increased cervical cancer risk. (AACR Journals)
The “selfish” part of this habit is rarely intentional. It usually shows up as:
-
Smoking in the house, on the balcony, or near open windows, assuming it’s “good enough”
-
Brushing off complaints with “I only smoke a few”
-
Promising to quit without a plan, then repeating the cycle
-
Treating smoking as personal freedom rather than a shared home-health issue
What to do instead:
-
Make the home truly smoke-free. Not “sometimes,” not “by the window.” A clear household rule is the simplest protection.
-
Turn quitting into a shared project. If one partner wants to stop, the other partner’s support (and reduced exposure) matters.
-
Use structured help. Nicotine replacement, counseling, quitlines, or clinician support increases quit success compared with willpower-only attempts.
If you want one bottom-line principle: protecting cervical health isn’t only about clinics—it’s also about what happens in living rooms, kitchens, and shared air.
Habit 3: Putting Screening Off and Avoiding Follow-Up
:max_bytes(150000):strip_icc()/GettyImages-1396446063-712f314b87204164935931a6cad39b86.jpg)
Screening is one of the biggest reasons cervical cancer rates have dropped where access is strong. Many early cervical cell changes do not cause symptoms, which is why relying on symptoms is a trap. (World Health Organization)
But in real marriages, screening gets delayed for very “normal” reasons:
-
Busy schedules and childcare logistics
-
Fear of discomfort, fear of results
-
A partner minimizing it: “You’re fine. You look healthy.”
-
Lack of practical support (transportation, time off, budget priorities)
In a relationship, neglect often looks like absence of support, not active sabotage. And that’s exactly why it’s fixable.
What to do instead:
-
Make screening non-negotiable like dental checkups. Boring is good. Routine is protective.
-
Know the general guideline ranges (then confirm with local medical guidance):
-
Ages 21–29: Pap testing every 3 years (typical recommendation)
-
Ages 30–65: options include primary HPV testing every 5 years, Pap every 3 years, or co-testing every 5 years (depending on the guideline and availability) (ACOG)
-
-
Offer concrete help: schedule together, handle errands, watch kids, drive, and—most importantly—support follow-up if an abnormal result appears.
The goal isn’t to create anxiety. It’s to prevent a preventable disease by doing the unglamorous, repeatable things that work.
The Real Takeaway for Couples
Calling these “husband habits” can be attention-grabbing, but it also risks turning a health topic into blame. A better framing is this:
Cervical cancer prevention works best when couples act like a team—taking HPV seriously, protecting the home environment, and treating screening as routine health maintenance.
If you want a simple checklist for a household:
-
HPV prevention is discussed openly, not avoided
-
The home is smoke-free
-
Screening is on the calendar, and follow-up is supported
That combination does far more than fear-based warnings ever will.
Sources
-
U.S. National Cancer Institute — Cervical Cancer Causes, Risk Factors, Prevention (National Cancer Institute)
-
WHO — Cervical Cancer Fact Sheet (World Health Organization)
-
American Cancer Society — Cervical Cancer Screening Guidelines (American Cancer Society)
-
AACR (Cancer Epidemiology, Biomarkers & Prevention) — Smoking/Passive Smoking and Cervical Cancer Risk (AACR Journals)