How Male Fertility Changes With Age: What Medical Science Really Shows
For a long time, male fertility has been surrounded by a simple assumption: men can have children at any age without meaningful biological consequences. While it is true that men often remain fertile much longer than women, modern medical research paints a more nuanced picture. Age does affect male reproductive health—sometimes in subtle ways that are easy to overlook.
Understanding these changes does not mean discouraging older men from becoming fathers. Instead, it allows for informed decisions, realistic expectations, and better health planning.
Fertility Does Not Disappear — It Evolves
Unlike female fertility, which declines sharply after a certain age, male fertility typically changes gradually. Many men in their 40s, 50s, and even beyond are capable of fathering children. However, doctors emphasize that fertility is not just about the ability to conceive—it is also about sperm quality, genetic stability, and overall reproductive health.
From a medical standpoint, fertility involves multiple factors working together. Sperm count is only one piece of a much larger puzzle.
Sperm Count vs. Sperm Quality
One reason male aging effects are often underestimated is that sperm count can remain within normal ranges for many years. Standard fertility tests may show numbers that appear healthy, giving the impression that everything is unchanged.
However, urologists and reproductive specialists point out that quality matters just as much as quantity.
As men age, sperm may experience:
-
Reduced motility (the ability to swim efficiently)
-
Changes in shape and structure
-
Decreased ability to penetrate and fertilize an egg
Even small declines in these areas can influence conception success, especially when combined with other health factors.
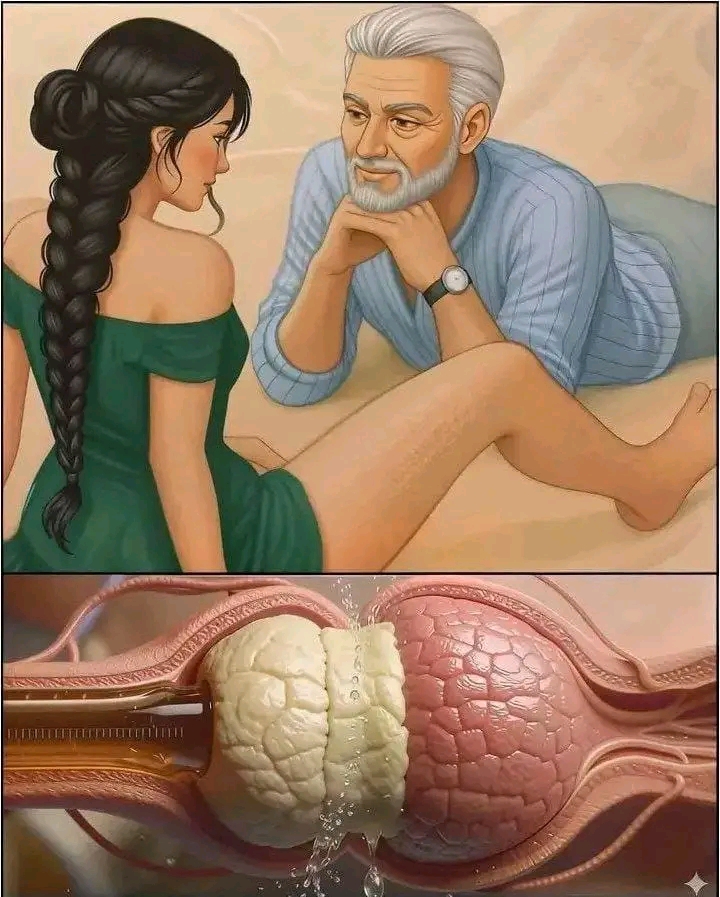
Why Sperm Motility Matters

Sperm motility refers to how effectively sperm move through the female reproductive tract. This movement is essential for fertilization. Research indicates that aging sperm may move more slowly or less directly, reducing the likelihood of reaching the egg.
This does not mean conception is impossible. It means that the process may take longer or require more careful planning. In some cases, couples may not realize sperm motility is an issue until they experience delays in achieving pregnancy.
DNA Integrity: A Quiet but Important Change
One of the most discussed age-related changes in male fertility involves DNA fragmentation. This term describes small breaks or irregularities in the genetic material carried by sperm.
Medical studies have shown that sperm DNA becomes more vulnerable to fragmentation with age. While many embryos can still develop normally, higher levels of DNA fragmentation have been associated with:
-
Lower fertilization efficiency
-
Increased risk of early pregnancy loss
-
Greater likelihood of requiring fertility support in some cases
It is important to note that increased risk does not mean inevitability. Many men with higher DNA fragmentation still father healthy children. The key message from doctors is awareness, not alarm.
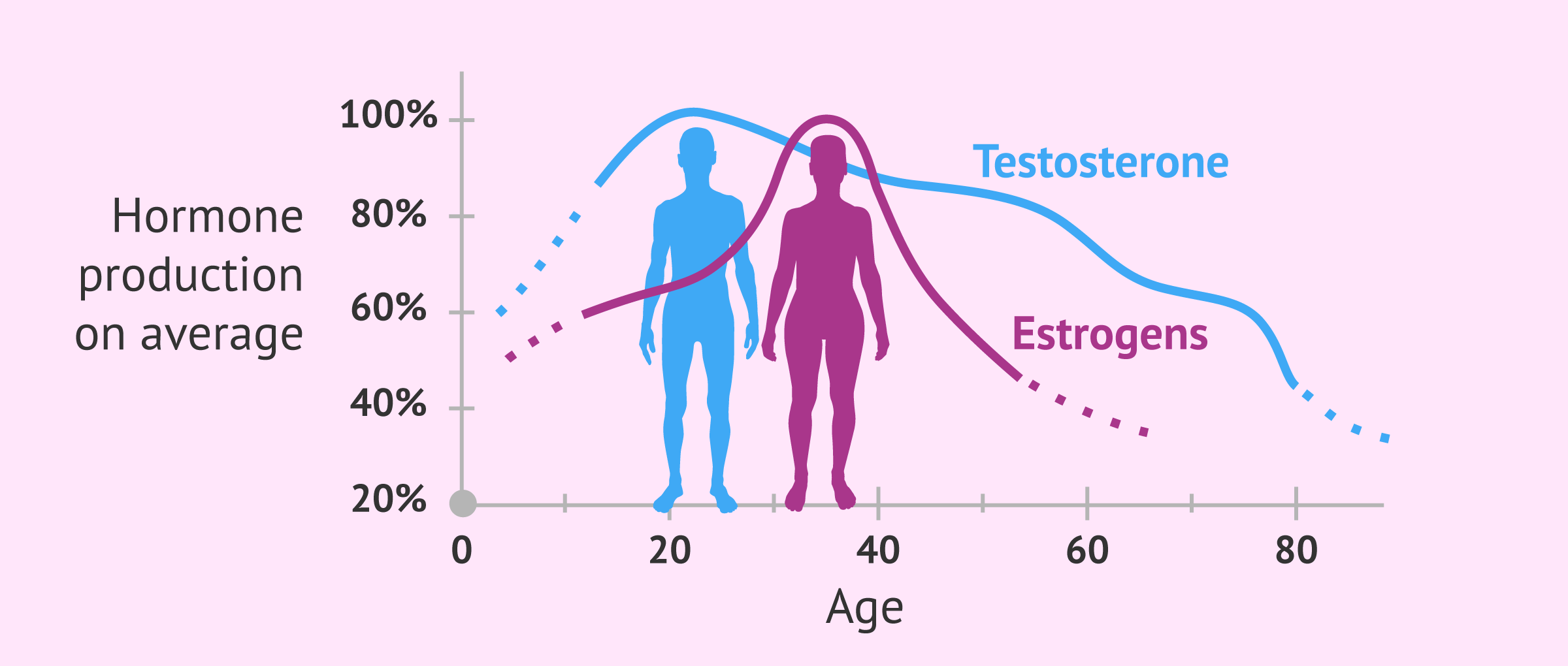
Hormonal Changes Over Time

Hormones play a central role in male reproductive health, and aging naturally influences hormonal balance.
Testosterone levels tend to decline gradually with age. This process is often slow enough that men may not notice immediate symptoms. However, testosterone influences more than libido—it supports sperm production, muscle mass, energy levels, and metabolic health.
Lower testosterone may contribute to:
-
Reduced sperm production efficiency
-
Changes in sperm maturation
-
Shifts in overall reproductive function
Lifestyle factors can either accelerate or slow these hormonal changes.
Lifestyle Factors That Amplify or Protect Fertility
Age alone does not determine reproductive health. Lifestyle choices have a powerful influence on how sperm ages.
Doctors consistently identify several factors that significantly affect sperm quality:
Sleep and Stress
Chronic sleep deprivation and long-term stress can disrupt hormonal regulation. Elevated stress hormones interfere with testosterone production and sperm development.
Body Weight and Metabolism
Excess body fat is linked to hormonal imbalance, inflammation, and reduced sperm quality. Maintaining a healthy weight supports more stable reproductive function.
Smoking and Alcohol
Smoking has been shown to damage sperm DNA and reduce motility. Excessive alcohol intake affects hormone levels and sperm production over time.
Nutrition
Antioxidant-rich diets—containing fruits, vegetables, healthy fats, and adequate protein—help protect sperm from oxidative stress, a major contributor to DNA damage.
Men who maintain healthy habits often preserve better sperm quality well into later adulthood compared to those with poor lifestyle patterns.
Advanced Paternal Age and Child Health: What Research Says

Medical research has explored links between advanced paternal age and certain developmental outcomes in children. Studies suggest that as paternal age increases, there may be a slightly higher statistical association with some conditions.
It is essential to emphasize context:
-
The overall risk remains low
-
Most children of older fathers are born healthy
-
Age is one factor among many, not a determining cause
Doctors present this information to support informed family planning, not to create fear. Understanding potential risks allows couples to make decisions based on knowledge rather than assumptions.
Fertility Testing: A Tool for Clarity
Many men do not consider fertility testing unless they encounter difficulty conceiving. However, reproductive specialists increasingly recommend proactive assessment for men who plan to delay fatherhood.
Fertility evaluations may include:
-
Semen analysis (count, motility, morphology)
-
Hormone level testing
-
DNA fragmentation assessment when appropriate
Testing provides objective data and can identify issues early, when lifestyle changes or medical support may be most effective.
Age Is Not a Deadline
Aging does not eliminate male fertility. It reshapes it.
This distinction is crucial. Men are not working against a fixed expiration date, but they are navigating gradual biological shifts. Understanding those shifts allows for smarter decisions about health, timing, and medical support when needed.
Doctors stress that many fertility-related challenges respond well to early intervention and healthy living.
What Medical Professionals Want Men to Know
Across specialties, healthcare providers emphasize several key points:
-
Fertility involves quality, not just the ability to produce sperm
-
Aging affects reproduction gradually, not suddenly
-
Lifestyle choices significantly influence outcomes
-
Awareness leads to better planning and better health
Rather than viewing fertility as something that either exists or disappears, experts encourage men to see it as a dynamic system that benefits from care and attention.
Listening to the Body’s Signals
The body often gives subtle signals long before significant problems develop. Fatigue, hormonal changes, weight gain, or shifts in sexual health can all reflect underlying changes in reproductive physiology.
Paying attention to these signals—and seeking medical guidance when needed—is a practical advantage, not a sign of weakness.
A Balanced Perspective on Male Aging and Fertility
Male fertility does not follow a dramatic cliff, but it does not remain static either. Modern science offers clarity where assumptions once prevailed.
For men considering fatherhood later in life, knowledge is the most valuable tool. With healthy habits, medical awareness, and proactive care, many men continue to support successful, healthy pregnancies well into later adulthood.
Aging changes fertility—but understanding those changes empowers better choices for the future.